PREFINAL PRACTICAL EXAM 1801006156

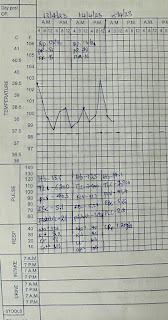
PREFINAL PRACTICAL EXAM 45 year old Female, farmer by occupation came to medicine OPD with chief complaints of Fever since 5 days Loose stools 2 days back HISTORY OF PRESENTING ILLNESS:- Patient was apparently asymptomatic 5 days back then she developed low grade fever which was insidious in onset and intermittent in nature associated with chills and rigor. Loose stools 2 days back ,4 episodes liquid in consistency ;not associated with blood. Weakness since 5 days. History of dry cough since 4 days. No history of burning micturition. No history of pain abdomen. No history of intake of outside food. No history of pain abdomen. No history of vomiting. No history of toddy drinking. DAILY ROUTINE:- Patient wakes up at 7 AM and does her household work and have breakfast around 9 AM and goes to work at agriculture land for 3 hrs and comes back between 12-1 PM and have lunch at 2PM, takes rest for the day. Patient have dinner at around 8PM and goes to sleep at 9PM.She takes rice with