35 years male patient with vomiting , generalised weakness and hiccups
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input. This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome. I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
Shaik sameer
Roll no 204
Chief Complaints-
35 year old male lorry driver by occupation resident of chitiyal came to opd with chief complaints of
Vomiting since 3 days
Hiccups since 3 days
Cough since 3 days
Loose stools for 1 day 3 days back
HOPI- patient was apparently asymptomatic 3 days back then he had vomiting which was sudden in onset, 10-15 episodes per day,non bilious,non projectile,food and water as the contents
Vomiting is present immediately after food water and alcohol intake which is associated with generalised weakness for which he went to local hospital in chityala and he was under saline infusion.
Loose stools- 4 episodes lasted for 1 day 3 days back
Non blood stained,large volume not associated with pain abdomen and fever, black coloured stools
Hiccups Since 3 days continuously, associated with mild difficulty in swallowing
Cough- dry since 3 days not associated with fever sore throat cold.
Past history:
H/o yellow discolouration of eyes associated with vomitings 5-6 episodes per day non bilious containing food particals 3 months back for which he went to local hospital and diagnosed as jaundice and treated for it.
Not a known case of HTN, DM, TB, Asthma, Epilepsy, CAD
No h/o any previous surgeries
No known allergies
Personal History
Diet- mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- regular
Addictions- chronic alcoholic since 16years (minimum 90ml per day) ,3 months back he has stopped Consuming alcohol as he was diagnosed with jaundice, but 5-10days back he again started consuming alcohol.
Increased consumption during night after dinner
Occasional toddy consumer
And also consumes tobacco in the form of gutka (betel quid). At first he used to take 1 packet per day now he is taking 10 packet per day
Family history
Not significant
General physical examination-
Patient is conscious coherent cooperative well oriented to time place and person moderately built and nourished
Pallor -absent
Icterus- absent
Cyanosis- absent
Clubbing absent
Lymphadenopathy-absent
Edema- absent
Vitals
Temperature- afebrile
RR-16/min
PR 75bpm
BP 130/70
Systemic examination-
Abdominal examination
On Inspection
Abdomen flat
No distension
Umbilicus is central
No engorged veins
No visible pulsations
No scars
Flanks are full
All inspectory findings are confirmed in Palpation
No tenderness
No guarding rigidity
No Hepatomegaly
No splenomegaly
Percussion-
Liver span 7cm
Auscultation-
Bowel sounds are heard
Respiratory system-
Trachea is central
B/l air entry is present
Normal respiratory movements
Normal vesicular breath sounds
Cardiovascular system-
S1 and S2 heard no murmurs present
CNS examination
No focal neurological deficits
Provisional diagnosis
Alcoholic liver disease
Hyponatremia
Acute kidney injury
Investigations
02/12/2022
LFT
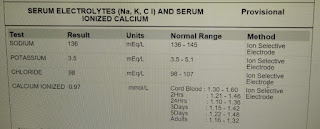
Serum electrolytes
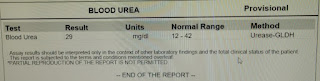
Blood urea
Serum creatinine
Lipase-
Serum amylase-
Urine protein/creatinine ratio
Complete urine examination
03/12/2022
Complete blood picture
Serum electrolytes
LFT
Serum creatinine
Blood urea
Prothrombin time
04/12/2022
Complete blood picture
Serum electrolytes
5/12/22
LFT
SERUM ELECTROLYTES
BLOOD UREA
SERUM CREATININE
COMPLETE BLOOD PICTURE
Other investigations
Chest x ray
USG abdomen
Treatment1. IVF- 0.9 NS @ 100 ml/hr
RL- @ 100 ml/hr
2. Inj. Thiamine 200 mg in 100 ml NS IV/TID
3. Inj. Zofer 4 mg/ IV/ TID
4. Inj. Metoclopramide 10 mg/IV/SOS
5. Syp. Lactulose 30 ml/ PO/ HS
6. Tab. Udiliv 300 mg PO/BD
7. Inj. Vit K 20 mg IV/STAT (100 ml NS) followed by Inj. Vit K 10 mg in 100 ml NS/IV/BD
8. Syp. Mucaine gel 15 ml/PO/TID
9. Tab. PAN-D (40/30) PO/OD
10.Strict I/o charting
































Comments
Post a Comment